Toe spacers and plantar fasciitis

Athletes play inordinate amounts of stress on their feet and improper footwear and foot strength can lead to injuries. But if you’re constantly dealing with stabbing heel pain, it may not be because of your shoes. You may be dealing with plantar fasciitis.
For anyone that’s ever dealt with heel pain, you know it’s not pleasant. You’re shocked with a stabbing pain when you walk that tends to disappear as you get moving. While you may chalk it up to poor shoes or lack of cushioning, the real reason you should be feeling pain in your heels is because of a condition called plantar fasciitis.
Plantar fasciitis is one of the most common causes of heel pain in adults and affects more than two million people nationwide. Your heels undergo a lot of wear and tear with daily activities and can lead to excessive pressure on your feet, which can subsequently damage or tear the ligaments. The result is inflammation of the plantar fascia, which results in heel pain and stiffness.
However, recent research suggests that the name plantar fasciitis should actually be replaced with plantar fasciosis because of the chronicity of the disease and evidence showing degeneration rather than inflammation.
Whether you’ve dealt with plantar fasciitis or know someone who is, we’re breaking down everything you need to know about the condition and giving you some of the best natural fixes that don’t include surgery—including toe spacers for plantar fasciitis.
Our 4-loop Toe Spacers, 5-loop Toe Spacers, and Toe Spacer Flex gently stretch the toes, foot muscles, and plantar fascia to support natural alignment and help ease tension associated with plantar fasciitis. You can check them out here, also keep reading to find out more about plantar fasciitis below.
What is plantar fasciitis?
The structure of the foot houses a thick band of dense, fibrous tissue called the plantar fascia. It runs from the heel to the toes and functions provide static support for the longitudinal arch and dynamic shock absorption. People who struggle with flat feet (pes planus) or high arches (pes cavus) have a higher risk of developing plantar fasciitis than people with normal arches.
When this band of tissue becomes inflamed due to excessive pressure, it results in plantar fasciitis.
The pain associated with plantar fasciitis is usually caused by collagen degeneration where the plantar fascia attaches to the medial tubercle of the calcaneus (heel bone). This type of degeneration is similar to that seen in chronic necrosis of tendonosis, which is characterized by a gradual loss of collagen, increases in ground substance (matrix of connective tissue) and vascularity, and the presence of fibroblasts as opposed to the inflammatory cells that are characteristic of acute inflammation of tendonitis. The primary cause of collagen degeneration is repeated microtrauma to the plantar fascia that overcomes the body's ability to repair itself.

Image source: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3951039/
Signs and symptoms
The primary complaint of people dealing with plantar fasciitis is stabbing pain in the heels or sometimes at the bottom mid-foot. Although plantar fasciitis is typically unilateral in nature, meaning it only affects one foot, it’s not uncommon that it affects both.
For most people, plantar fasciitis pain is most severe with the first few steps in the morning and will lessen as activity continues. Some people may also experience pain when standing for prolonged periods, which may be accompanied by stiffness. For others, severe pain may return toward the end of the day.
If you’re experiencing any of these, you could be dealing with plantar fasciitis:
- Pain on the bottom of the heel
- Pain in the arch
- Pain that’s worse in the morning (and sometimes at night)
- Pain that increases over a period of months
- Swelling on the bottom of the heel
What causes plantar fasciitis
The most common reason why plantar fasciitis develops is because of the faulty structure of the foot. People who have arch deformities—either collapsed arches or high arches—are at an increased risk of developing plantar fasciitis.
However, most people who develop plantar fasciitis have faulty biomechanics that causes abnormal pronation of the foot. Here’s an example. Someone with a flexible rearfoot varus (foot is inverted relative to the ground) may appear as if they have a normal foot structure but when bearing weight, may actually display significant pronation. The ankle will plantarflex and adduct as the period stands, while the heel everts or rotates outward. As a result, tension increases on the plantar fascia.
Some other conditions that can cause abnormal pronation forces to include:
- Tibia vara
- Ankle equinus
- Rearfoot varus
- Forefoot varus
- Compensated forefoot valgus
- Unequal limb length
Increased pronation is a major contributor to plantar fasciitis because it places additional stress on the centre of the band. And since the weakest point of the plantar fascia is the origin—not the substance—you’re further weakening it and increasing the risk of injury.
Risk factors for plantar fasciitis
Both intrinsic and extrinsic factors may play a role in the risk of plantar fasciitis. These include:
Intrinsic
- Anatomic
- Obesity
- Flat feet
- High arches
- Shortened Achilles tendon
- Biomechanic
- Overpronation
- Limited ankle dorsiflexion
- Weak intrinsic foot muscles
- Weak plantar flexor muscles
Extrinsic
- Environmental
- Poor foot biomechanics or alignment
- Deconditioning
- Hard surface
- Walking barefoot
- Prolonged periods of weight-bearing
- Insufficient stretching of the feet
- Inappropriate footwearPlantar fasciitis fixes
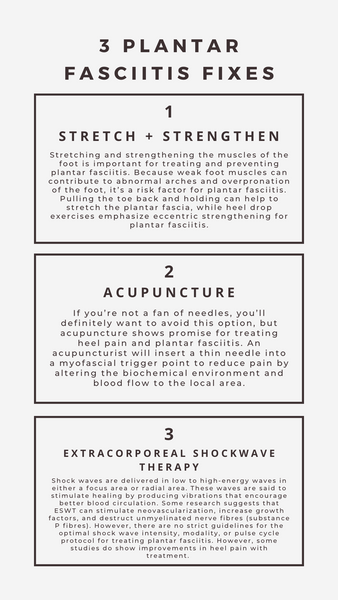
Plantar fasciitis fixes
While addressing the inflammatory component of plantar fasciitis and patient discomfort is important, education is perhaps even more so. Education to understand the etiology of pain, including biomechanical factors that cause symptoms, can help people learn about home therapies that may relieve some pain and discomfort. It also helps them to understand how simple changes in their daily activities can make a massive contribution to reducing the likelihood of development or recurrence.
Some of the nonoperative treatments for plantar fasciitis can be helpful, however, many of them—orthotics, taping, night splints—are not actually getting to the root of the problem. With that said, here are some that you may find beneficial:
Toe spacers and plantar fasciitis
While surgery may be the go-to option for some people, there’s a much easier way to prevent plantar fasciitis from happening in the first place—toe spacers.
Plantar fasciitis can be a complex and tricky condition to treat where treatment options can really vary in efficacy. One thing that can be really bad for plantar fasciitis is weak, inflexible feet that result from being crunched up in poorly fitting shoes day in and day out.
This is where toe spacers shine.
Two major issues that contribute to the development of plantar fasciitis are poor foot mechanics and reduced blood flow—both of which wearing toe spacers can address.
Spending countless hours in shoes that are too small, too tight, or uncomfortable leads to dysfunctional feet. The toes are squished together leading to misalignment. Bodyweight is shifted forward to the balls of the feet. And muscles are not given an opportunity to activate and do what they’re meant to do. The result is a foot that doesn’t function as it should.
On top of that, modern running shoes impair blood supply. If you look at the natural shape of a foot, it’s widest at the toes—not the balls. When you put on shoes that pull the toes upwards, you’re putting stress on the muscles that help move your toes. That movement, in turn, pinches the arteries that supply blood, which means that blood flow is impaired to the region where plantar fascitis pain tends to occur. Essentially, the junk never gets flushed out of the feet and starts to cause problems.
Conventional treatment for this condition focuses on treating the wrong part of the foot. Instead, they need to be putting the toes back to the position they were meant to be in.
While there’s little scientific evidence on the role of toe spacers in treating plantar fasciitis, there is research showing the benefit of them in strengthening intrinsic foot muscles and realigning the body toe. So, when you can fix the factors that contribute to the development of plantar fasciitis, you drastically reduce your odds of developing it.
If you want to learn more about how you can treat and prevent plantar fasciitis, check out our training program. It delivers long-term solutions to strengthen your feet by providing temporary relief. The Plantar Fasciitis Training Program is a 12-week program delivered via PDF that can be used interactively on your phone, laptop, or tablet.
What's included:
- Anatomy overview
- 12-week program with a terminology cheat sheet
- Video explainers and detailed tutorials
- 3-4 60-minute sessions per week with optional daily mobility
- A set of Toe Spacers
Check out the program here>
Resources
Barrett SJ, O'Malley R. Plantar fasciitis and other causes of heel pain. Am Fam Physician. 1999;59(8):2200-2206.
DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A(7):1270–1277.
Rathleff MS, Mølgaard CM, Fredberg U, et al. High-load strength training improves outcome in patients with plantar fasciitis: a randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2015;25(3):e292–e300.
Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J. 2014;18(1):e105-e107. doi:10.7812/TPP/13-113
Trojian T, Tucker AK. Plantar Fasciitis. Am Fam Physician. 2019;99(12):744-750.